As Patrick Grohar, PhD, MD at Children’s Hospital of Philadelphia puts it, “[Osteosarcoma] is very complicated, and will take a lot of experts, working together to solve the problem”.
With cancer models, molecules, canines, and colleagues, he created an innovative plan to make new treatments for children with osteosarcoma who don't respond to current therapies and need a different way to survive.
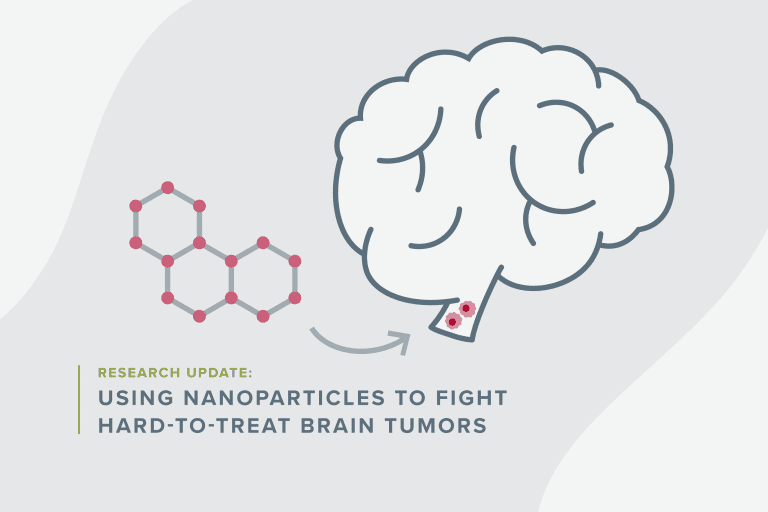
Using The Fight Osteosarcoma Together (FOT) Super Grant, funded in part by the Zach Sobiech Osteosarcoma Fund, Dr. Grohar will spend three years leading a research team to investigate a family of genes called MYC. His larger goal is to identify targeted treatments for osteosarcoma patients whose MYC genes have gone awry.
Dividing osteosarcoma into subtypes, so it's easier to target
Unlike many sarcomas, osteosarcoma has a number of different genes from patient to patient that drives growth. Current treatments try to squelch all the bad genes at once, but certain mutations find a way around them.
Dr. Grohar has spent most of his career studying Ewing sarcoma, a bone cancer that grows because of a main-driver mutation called EWS-FLI1. Ewing sarcoma has a well-established driver, but researchers struggle with treatment for this tumor as well. His research in Ewing sarcoma sparked an idea, a new way to approach the complicated bone cancer.
“Another way to think about osteosarcoma,” he said, “is that it’s not that different [than other bone cancers.] The difference is that it’s a collection of diseases with defined genomes.” Using his findings with Ewing sarcoma, he wondered if approaching osteosarcoma like several sub-type diseases instead of one giant, snarled disease could help target recurring, high-risk osteosarcoma better.
According to Dr. Grohar, the scientific literature shows that a genetic change called MYC-amplification occurs in 12-39% of the osteosarcoma population and is linked with poor outcomes. He thought this would be a good place to start to look for treatment targets.
“In the Children’s Oncology Group, we’ve talked about what’s next for osteosarcoma, and there’s a collective belief that molecular subtype therapy is the direction we’re headed,” he said.
Now, his team will work to explore MYC-amplified osteosarcoma and try to define its genome, asking questions like: Why is it connected to poor outcomes? Is MYC-amplification chemo-resistant? Is it causing osteosarcoma to spread? Is it both? By zooming in on MYC-amplification, they can expose its vulnerabilities and develop targeted compounds that specifically attack the mutation and the processes that allow it to grow. He knows no single researcher can answer these questions alone and that enacting a multi-pronged approach is imperative if they want to make progress quickly.
A collaborative approach
“We put together a really great team,” said Dr. Grohar, who has brought together experts from all corners of cancer research to study osteosarcoma MYC-amplification.
- MYC-amplification expert, Nouri Neamati, PhD studies MYC-amplification in other cancers and already has a compound he thinks could target MYC-amplified osteosarcoma. If his compound is successful in the lab, it could be ready for clinical trial in three years.
- Metastatic cancer expert, pharmaceutical company Vuja De Sciences has analysis technology that shows how metastases (cancer that spreads) develop and which steps in the metastatic process they could stop with targeted treatments. Since MYC-amplification is connected to high-risk, recurring osteosarcoma, information on how MYC contributes to cancer spread will be important.
- Memorial Sloan Kettering osteosarcoma expert, Filemon Dela Cruz, MD has a set of sarcoma mouse models he will be using to study MYC-amplification and subsequent targeted compounds
- Canine osteosarcoma veterinarian expert, Chand Khanna, DVM, PHD, DACVIM (ONC), DACVP (HON) will help Dr. Grohar set up a canine clinical trial with 18 dogs who have MYC-amplified osteosarcoma to test compounds.
MYC-amplification occurs in several other cancers, and Dr. Grohar is confident that his findings will be translatable to those diseases, too.
“This is a clear clinical need,” said Dr. Grohar. “There’s no question about it. We didn’t have the resources to go at it in the way that we needed to: To see something valuable in the clinic in a time frame that’s reasonable. That’s what’s great about this grant. It allows us to go all in, leverage our own resources, take the experience of others who have worked in MYC [and metastases], and bring them into the fold to think about this particular pediatric cancer. I’m really excited about it-- it’s a really cool project.”
Your donation funds researchers like Grohar.
Your support propels bold ideas forward and empowers researchers to discover treatments that are better and safer for kids, and ensure every child can have a long, healthy life after cancer.