Small things can snowball into something so much larger and more significant.
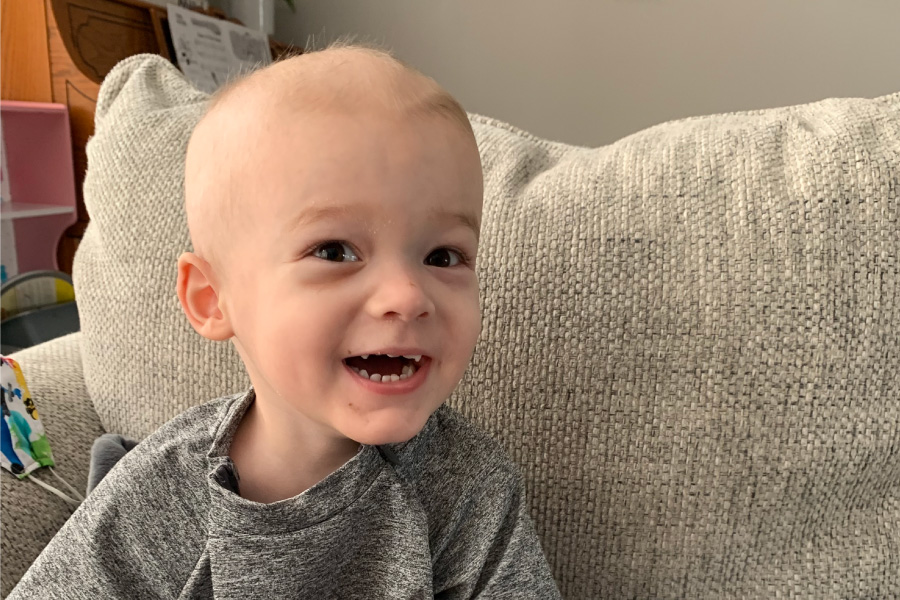
A genetic error while a baby is still in the womb triggers pre-leukemia cells that can later bloom into full-fledged leukemia. A tiny dried blood spot from a newborn heel stick could hold clues into how to prevent the disease. And philanthropic gifts launch a small research pilot project that eventually scales up into a much bigger, federally funded study.
Erin Marcotte, PhD, MPH, and Heather Nelson, PhD, MPH, of University of Minnesota are seizing the opportunity to turn small things into big hope for the future of childhood leukemia. In 2016, the pair received a grant from Children’s Cancer Research Fund (CCRF) to develop a new method to predict which children are at risk of developing acute lymphoblastic leukemia (ALL) — and perhaps one day prevent it.
“CCRF really took a chance on our idea and believed in our vision and what it would mean for the field,” Marcotte said. “It’s one of those projects that truly could revolutionize the way we think about childhood leukemia from a research perspective, but also potentially the number of kids who develop leukemia in the future. It’s difficult to overstate the promise of this, and I’m very excited to be on the ground level working on this project and having the support from CCRF and our other funders.”
The researchers’ results from that initial CCRF-funded study recently helped them secure a five-year, $3.5 million grant from the National Institutes of Health (NIH) — a larger-than-usual grant for this kind of project.
“I can honestly say this research would not have happened without CCRF,” Nelson said. “We are really grateful that CCRF invested in this project because without their support, we would not have gotten to this next big step.”
Understanding pre-leukemia
Past research on cancer patients has shown that pre-leukemia genetic mutations can be present at birth — even if the child isn’t diagnosed for a decade or more. Nelson and Marcotte are focused on a specific gene fusion known as ETV6-RUNX1, which has been found in newborn blood samples of more than 60 percent of children who were later diagnosed with ALL.
“We know that every cancer is unique,” Nelson said. “That makes it very difficult to have a single laboratory assay that will detect every cancer. What we have developed with CCRF support is a laboratory method that will detect the most common genetic error in childhood leukemia, and we can use that to screen for the presence of pre-leukemia at birth. It’s not perfect, because again every cancer is unique, but if we can detect the majority of pre-leukemia at birth, that is a big breakthrough.”
But just as significant are the many children who are born with pre-leukemia but never go on to develop the disease. While the exact number is still unknown, researchers believe that pre-leukemia is much more common than the relatively rare childhood leukemia rates.
“We have to figure out what happens after birth to protect some kids from developing leukemia,” Nelson said. “That can only happen if we can measure pre-leukemia at birth.”
A better way to screen
Previous research in the field focused on healthy children using umbilical cord blood samples, but Marcotte and Nelson were convinced that there was a better way. Instead, they turned to newborn dried blood spots, which are routinely collected and easily stored. All newborns born in the United States and in many other parts of the world have the standard heel stick test to screen for various diseases.
The challenge was detecting where the pre-leukemia genetic error occurred. Researchers can pinpoint the change when looking back at the newborn dried blood spots of leukemia patients, but without later leukemia cells for comparison, they have to know where to look.
Using advanced genetic sequencing, Nelson and Marcotte developed a method called breakpoint agnostic translocation screening to detect ETV6-RUNX1 in children who had not yet developed cancer. Their method is also able to detect very rare events — like a single pre-leukemia cell that might be hidden among 5,000 normal cells. Then they tested their method in 60 newborn dried blood spots from healthy children and those with leukemia.
“NIH would not have funded our project without proof that we had a laboratory assay that could measure pre-leukemia,” Nelson explained. “CCRF funded the development of the method; NIH is now taking the baton and funding the work that tells us who does and does not have pre-leukemia at birth. The next step will be to figure out when pre-leukemia goes away and when it progresses to a leukemia diagnosis. And once we know that, we can prevent a significant portion of leukemia.”
Working toward new prevention tools
But first, they need to understand which factors increase a child’s likelihood of developing ALL. As part of the NIH project, Marcotte and Nelson will test their method on newborn dried blood spots from 3,000 healthy children and 500 children with leukemia. It’s the largest study of its kind so far and also one of the most diverse data sets.
“We know that the incidence rates of ALL vary dramatically by race and ethnicity, and we are wondering whether the translocation frequency at birth underlies these disparities,” Marcotte said. “For instance, Hispanic children are 45 percent more likely to be diagnosed with childhood leukemia than non-Hispanic white children. Is some of that due to a higher rate of pre-leukemia at birth? We have no idea because no one’s ever looked in that population, and we intend to.”
Race and ethnicity are just one facet they plan to explore. In collaboration with Margaret Karagas, PhD, director of Children’s Environmental Health and Disease Prevention Research Center at Dartmouth, they will test newborn dried blood samples from 1,000 children in the New Hampshire Birth Cohort Study. Karagas then will follow the children who have pre-leukemia to see if the cells are still detectable over time.
While the research team is starting with the most common subtype of ALL, it’s possible that their work could be expanded to other subtypes of ALL as well as acute myeloid leukemia (AML).
A future without childhood leukemia
It might take a decade or two before leukemia screening could be widely adopted, but the research is already attracting attention. Marcotte presented their work at the International Workshop on the Causes of Childhood Leukemia in Germany in 2022 and at the inaugural Childhood Cancer Prevention Symposium in Washington, D.C., in October 2023.
It’s an exciting time to work in childhood leukemia prevention, Marcotte noted.
“I hope within my career and my lifetime, I see some of this work coming to fruition,” she said. “To prevent even a handful of these children and families from going through a leukemia diagnosis and dealing with not only the acute impacts of treatment, but also the long-term health impacts these children encounter for the rest of their lives, would be absolutely incredible.”
Your donation funds researchers like Marcotte and Nelson.
Your support propels bold ideas forward and empowers researchers to discover treatments that are better and safer for kids, and ensure every child can have a long, healthy life after cancer.