It’s a ritual that has become familiar at Children’s Hospital of Philadelphia (CHOP) and other hospitals across the nation: the ringing of a bell to signal that a patient has finished cancer treatment.
But what happens after the bell rings? And how can cancer clinics get survivors — particularly in the adolescent and young adult years — to commit to critical follow-up care?
Those questions drive CHOP psychologist Dr. Lisa A. Schwartz’s research on how to improve self-management in cancer survivors ages 15-29. With support from Children’s Cancer Research Fund (CCRF), Schwartz is leading a pilot study to explore why adolescent and young adult (AYA) survivors may be disengaged from cancer-related follow-up care and to develop interventions that target reasons for disengagement.
The need for ongoing care
Thanks to treatment advances in recent decades, the population of survivors continues to grow. “Childhood cancer has a happy ending most of the time, but it leaves a whole other chapter in somebody’s life that presents a challenge, that is the need for continued multidisciplinary follow-up care,” Schwartz noted. “We want be able to target survivors early and use it as a teachable moment to say, ‘This is something you have to do every year for the rest of your life.’”
Schwartz is especially intrigued by the behavioral and psychosocial factors affecting survivors in the adolescent and young adult years, when survivors develop some autonomy over their health care. “The idea of focusing on AYAs who survive cancer and have this medical challenge on top of developmental challenges in a vulnerable time — that drew me in,” she said.
Learn more: Reaching More Milestones - The Importance of Survivorship Care
Nationally, more than half of adult survivors of childhood cancer are what’s known as “lost to follow-up,” meaning they don’t come back for annual follow-up care. That’s a problem because regular check-ins with an oncologist can help catch cancer relapse early and maximize quality of life for survivors by managing late and long-term side effects.
Learn more: CCRF introduces new research grant focused on cancer survivorship
“We’re really interested in re-engaging those survivors who have not come back for annual follow-up care, and this has recently been identified as a health disparity issue at the national level,” Schwartz noted.
Understanding patient barriers
In 2021, a report from the National Cancer Institute highlighted the need to address disparities among childhood cancer survivors. Research has found that survivors from marginalized backgrounds, who have lower income levels, or who live farther from a cancer center are less likely to engage in follow-up care.
“I think it’s a really great opportunity to start to work on this problem of addressing disparities,” Schwartz said. “I’m excited to quickly be able to contribute and hopefully make a difference clinically for these patients who we’re really invested in getting back so we can keep them healthy.”
What keeps patients from returning is a multi-faceted issue, she noted.
“There are aspects of the patient, the parents, the hospital system, and policy in general that are probably influencing those cases,” she said. “We want to reach out to those who are not engaged in care, find them and ask: What are the barriers? What can we do to help you? And I presume that for some it’s simply, ‘I forgot, I didn’t realize it was time to make my appointment.’ For others, it may be much more complex and layered, where they may need help with transportation or insurance, or there might be health literacy issues or trust issues. So, we want to identify those barriers and then create digital health tools to help address them.”
Read more: Sara's Story - What it Means to Survive
The power of a text message
Her primary tool to reach young people: the cell phones that are often their near-constant companion. Schwartz has led previous studies involving mobile apps and is the co-founder and co-director of CHOP’s Mobile Health Research Affinity Group. “I’m not a tech-savvy person trying to intervene with a very tech-savvy population,” she said with a laugh. “You have to think outside the box in terms of delivery of interventions that are mobile or digital in some way.”
For this project, Schwartz will spend the first year collecting data with patients and parents to better understand barriers to care. She’ll then develop intervention content targeting barriers, which will include adapting digital tools she used in prior interventions. After that, she’ll conduct a small pilot study evaluating the intervention with 75 survivors, ages 15-29, who are overdue for follow-up appointments at CHOP.
The planning stage is key. Schwartz will draw on behavioral economics — the study of how people make decisions — to explore how to best influence survivor behavior. “In theory, what those text messages say should be important,” she said. “There are different nuances to it. Not just, ‘Hey, you need to make an appointment,’ but does it matter if we tell them why they need to make an appointment? Like what they have to gain from it or what they have to lose from not coming back? Or does it make a difference if we give them discrete choices, like ‘We have these four appointment times available’? With this study, we get a little leeway to vet some of those options.”
Bringing new strategies into the clinic
If all goes as planned with the pilot project, Schwartz will then test the intervention with a larger population. “I’m so excited because ultimately we would want to do a more sophisticated trial and then implement this into the standard of care,” she said. “We want to be able to say: Who are the people that just need a nudge, like a text message, ‘Hey, time to make your appointment,’ versus who are the people who need more complex, tailored intervention? We believe we don’t need to implement high-resource interventions for everybody. This will give us a better window into low- and high-resource strategies that may work and that should be tested in a future trial.”
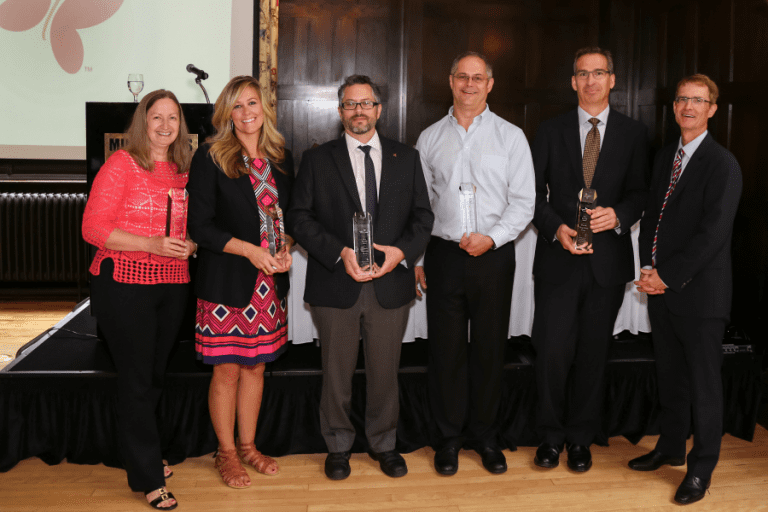
In the meantime, Schwartz is grateful to the donors who invest in pilot projects like this one. Approximately half of her grants come from foundations like CCRF, and the pilot data generated by those grants has laid essential groundwork for her larger, federally funded studies. “Philanthropy has been critical, especially in the work I do as a behavioral scientist,” she said. “When a foundation is supportive of the kind of work I do, that’s like a gold mine because sometimes it’s hard to get those grants from the National Institutes of Health or the CDC. I’m just so appreciative that CCRF is funding survivorship research, and not just survivorship research, but patient-oriented research. I’m grateful for this new opportunity.”
Support Groundbreaking Research
Your support propels bold ideas forward and empowers researchers to discover treatments that are better and safer for kids, and ensure every child can have a long, healthy life after cancer.